Providing Essential Health Services and Education
Providing Health Services and Education
Maternal and Child Health Nutrition Family Planning HIV/AIDS Polio TB Malaria

The majority of deaths in children under-6 years come from illnesses that are preventable or readily treatable. CHWs, trained in child survival, have found that pneumonia, diarrhea, meningitis, malaria, malnutrition and anemia can be recognized early, treated inexpensively and, with good counseling, prevented at the village level.
In India, pneumonia causes approximately 20% of mortality among children under 5. The prevalence of pneumonia is higher in rural villages. The common risk factor is poverty, malnutrition, low birth weight and the exposure to the burning of solid fuels in the home.
Anemia is widespread in rural populations particularly among expecting mothers and children. Extra care in identifying nutritional deficiencies and counseling on diet is key to lowering morbidity and mortality.
Community health workers focus on early detection, timely treatment and prevention of these common illnesses and depend on strong referral relationships with local government and private clinics, physicians and hospitals for fast treatment.
Maternal, Child Health, and Nutrition
Rural communities depend on CHWs for guidance on maternal and child health.
India has made great progress since 1990 in lowering the rate of maternal, infant and child mortality.
Despite these successes, we have fallen short of the Millennium Development Goal Target for 2015 by a wide margin and, when compared to a country like Indonesia (under-5 mortality 29 per 1000 live births), it is clear that a lot of work remains.
| 1990 |
2013 |
|
| Maternal mortality per 100,000 live births | 560 | 190 |
| Infant mortality per 1000 live births | 88 | 41 |
| Under-5 mortality per 1000 live births | 125 | 53 |
The challenge is even greater among the rural poor where maternal and child mortality is significantly higher. Poverty, low birth weight and malnutrition are the greatest risk factors determining the health of mother and child.



Community Health Workers (CHW) take on a variety of responsibilities; from treating simple illness and providing referral services for serious disease to delivering counseling and patient home care. CHWs have been important in promoting vaccinations for infants and children as well as institutional births.
Family Planning
In cooperation with local schools, community groups, and other NGOs

Over the past 25 years progress has been made in lowering the unmet need for family planning services. In 1990 the unmet need was 20%, in 2010 – 14%. In some populations of rural poor unmet need has been measured as high as 38%.
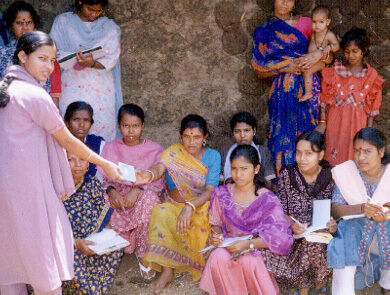
The challenges to meeting family planning needs are attributable to poverty, low literacy, lack of knowledge and lack of access. CHWs focus on education and partnering with programs that provide affordable family planning options for rural families. CHW’s are also active in expanding the definition of women’s health to include the broad spectrum of health issues relevant to women including, but not limited to, maternal, sexual and reproductive health.
HIV/AIDS
Community Health Workers are often the first person consulted in rural villages

In 2009 it was estimated that 2,400,000 people were living with HIV AIDS in India. 39% women. Over time, the HIV/AIDS epidemic has moved from urban to rural areas and from high-risk to the general population. The disease largely affects youth.
The national HIV/AIDS strategy entails integrating programs for prevention, support and treatment including peer led interventions by Non-Governmental Organizations and Community Based Organizations. These are linked to general healthcare facilities to ensure that there is access without stigma or discrimination. All are networked to Community Care Centers, Counseling and Testing Centers, and anti-retroviral treatment centers located in government hospitals.
These services are being expanded to Primary Health Centers in the rural areas, private sector facilities and mobile clinics.
In many rural areas local trained Community Health Workers and their local NGOs form the majority of the volunteer work force for government HIV/AIDS prevention and treatment initiatives like this AIDS Awareness Partnership with the local Lions Club promoting social mobilization and community engagement.

Polio
In rural areas, local NGOs powered by community health workers provide the woman and man power behind the Pulse Polio Program and are responsible for the eradication of the disease.

Until early 1990s India was hyperendemic for polio, with an average of 500 to 1000 children getting paralyzed daily. In 2014 the World Health Organization certified India as polio free. This marks one of the greatest achievements in public health.
Transmission was finally interrupted by sustained and extraordinary efforts. Since 2004 annual pulse polio vaccination campaigns were conducted 10 times each year, virtually every child was tracked and vaccinated. The elimination of polio has been dependent on the sincere work of countless health-workers, non-governmental organizations (NGOs), and local volunteers. In rural villages government polio workers have depended upon local village based health workers as the volunteers required for this effort.
In some communities the prevalence of post-polio paralysis was as high as 6/1000 preschool children. Decades of high prevalence of polio have left hundreds of thousands in need of continued help. Families have experienced not just the loss of healthy children but whole communities have experienced the disability-associated productivity loss associated with the disease.
Local community-based NGOs led by Community Health Workers have organized wheelchair distribution programs and have organized and assisted in polio reconstruction surgery camps with other NGOs and expert surgeons funded through the private sector.

Tuberculosis
Local trained CHWs are the 1st line of defense against an expanding threat of Tuberculosis in the community.

Tuberculosis remains a major public health problem in India, with the country accounting for 26% of all TB cases reported globally. Approximately 300,000 people die from TB each year in India.
The Government of India launched the Revised National Tuberculosis Control Program (RNTCP) in 1997 to provide free diagnostic and treatment services to benefit the poor and vulnerable groups of the society.
This national program, based on the internationally recommended Directly Observed Treatment Short-course (DOTS) strategy, has been shown to increase access to services for TB patients who are illiterate and from low-income rural households.
TB mortality and prevalence in the country has decreased compared with 1990 figures, indicating progress towards achieving TB-related targets of the United Nations Millennium Development Goals (MDGs).
Village based CHWs participate in local program efforts directly, through local NGOs, by providing awareness, detection, and treatment services as well as indirectly by counseling people with symptoms on where to get diagnoses and treatment.

